Drug decriminalization has not had more positive than negative outcomes in British Columbia, senior-level police told a House of Commons Committee, noting that while arrests for drug possession have decreased, overdose deaths have not declined.
The Standing Committee on Health heard from police and medical experts on April 15 regarding both the ongoing opioid crisis affecting parts of Canada and health-focused strategies to deal with drug addiction and overdose, such as the decriminalization of the possession of small amounts of illicit drugs in B.C.
Several senior police officials testified before the committee, including RCMP Deputy Commissioner Dwayne McDonald and Vancouver Police Deputy Chief Fiona Wilson.
Asked by Bloc Québécois MP Luc Thériault whether they believed the decriminalization of drugs in British Columbia had led to more positive than negative outcomes regarding the opioid crisis, both Mr. McDonald and Ms. Wilson said no.
“I would say there are positive results from decriminalization, as Deputy Chief Wilson has indicated, in terms of the number of people charged with criminal offences and attempts to divert them away from the criminal justice system. However, we do note challenges in public consumption and ancillary criminal behaviour,” Deputy Commissioner McDonald said.
He added that since decriminalization, overdose deaths and overdoses overall have not declined in B.C. What has decreased is the number of people being charged for simple possession of illegal drugs.
Deputy Commissioner McDonald also said police are having issues identifying safe supply drugs as many are diverted into the criminal marketplace and often cannot be identified as safe supply once out of their packaging. Criminal seizures of safe supply drugs have been made in communities like Campbell River and Prince George.
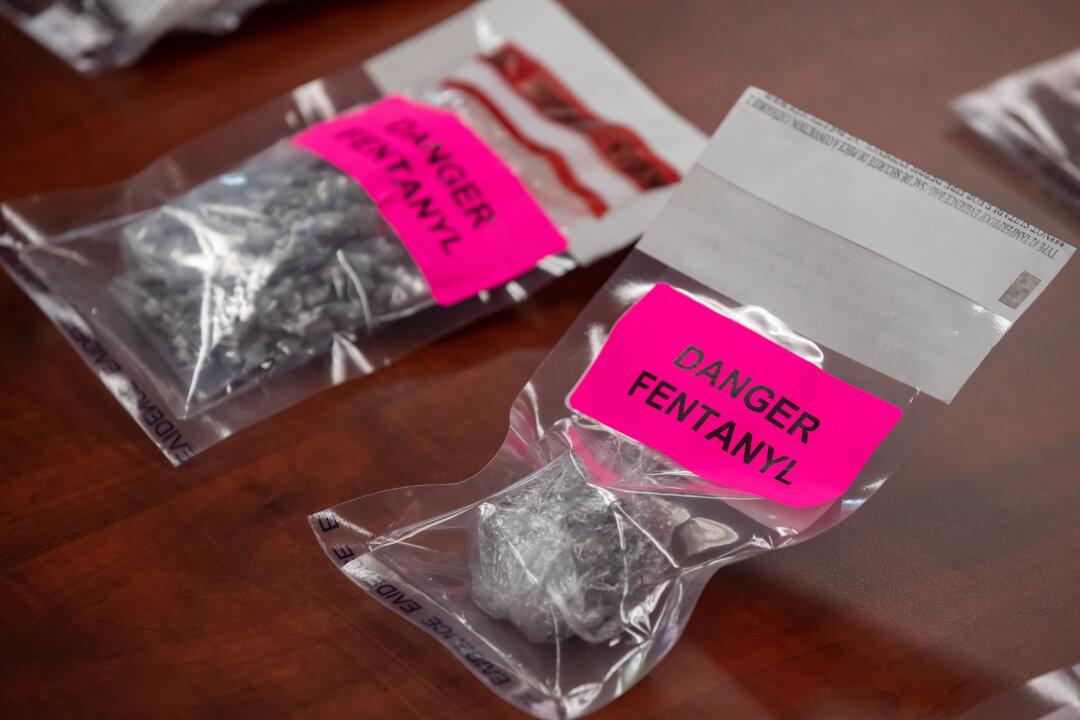
Vancouver Police Deputy Chief Wilson highlighted the growing toxicity of street drugs, saying that over the last 10 years there has been an “incredible toxicity” in the drug supply. She blamed widespread use of fentanyl, which she said accounted for 85 percent of overdose deaths in B.C.
In her opening statement to the committee, Deputy Chief Wilson said at least 14,000 people have died from accidental overdoses since the province declared a public health emergency regarding overdose deaths in April 2016.
She cited Vancouver’s Downtown Eastside as particularly serious. “Here, the stark reality is that the overdose crisis is more than 12 times the provincial average,” she said.
The British Columbia Association of Chiefs of Police, for which she serves as president, wanted the B.C. government to address potential consequences of decriminalization, such as impaired driving or public consumption.
“However, the implementation of decriminalization occurred before more fulsome restrictions on public consumption and problematic substance use could be adopted,” she said.
High-profile public drug use has occurred at parks, beaches, and public transit locations, she said. “In addition, there have been concerns from small businesses about problematic drug use that prevents access by customers or negatively affects operations.”
Illicit drug use in B.C. hospitals has also become a concern after a leaked Northern Health Authority memo called on hospital staff not to confiscate weapons or illegal drugs from patients.
The organization receives government funding, which it allegedly spent on illegal drugs that were to its clients.
Dr. Nathaniel Day, provincial medical director of addiction at Alberta Health Services, said his province is working to combat the overdose crisis by giving those in rural communities access to virtual health care. He touted the province’s virtual service for providing quick prescriptions and other help so patients can avoid withdrawal.
All of those testifying before the committee agreed that a health-focused approach is the ideal way to go about tackling the overdose crisis.